23.11.2020
The number of mental illness cases increases during viral epidemics. One hypothesis is therefore that the virus affects the brain in some way. Since it is not possible to examine the brain tissue of living people, Eleanor Coffey’s research team examines the blood, as the blood is the organ that directly communicates with the brain.
The number of mental illness cases increases markedly during epidemics, and there is a risk, albeit statistically small, that those who are exposed to the virus that causes COVID-19 can suffer from neurological damage and mental illness.
How do the diseases occur? What damage do they cause? How can one alleviate the long-term side effects? These are the questions that Eleanor Coffey, Research Director in Cell Biology at Åbo Akademi University and Vice Director of the Turku Bioscience Centre, has received funding from the Academy of Finland to investigate, along with her research group.
– Fortunately, the Academy of Finland made quick decisions, says Coffey.
The phenomenon of viruses causing mental illness has been observed since the 18th century in connection with epidemics and pandemics. During these epidemics and pandemics, the increased incidence of schizophrenia is particularly prominent. Mothers who are infected with a virus during pregnancy also have an increased risk of their children suffering psychological damage.
– This can be observed with the Spanish flu, SARS 1, SARS 2, and so on. Previous coronavirus epidemics in Asia have also given rise to mental illness.

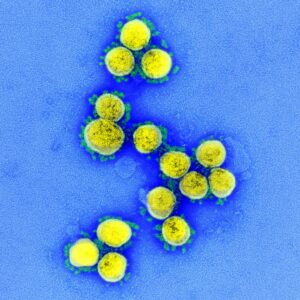
There is no clear knowledge of what causes the virus to result in mental illness. The presence of the so-called blood–brain barrier means that not everything in the blood actually reaches the brain, but it is still clear that certain types of molecules—in addition to the oxygen, glucose, and amino acids necessary for the brain—move between the bloodstream and the brain.
– It has recently been shown that the virus known as SARS-CoV-2 enters cells by binding to a protein on the cell membrane. The protein is called ACE2, and it has appeared in large amounts in the brains of virus-infected people who have shown brain-related symptoms.
Blood instead of brain tissue
One problem for this research is that, since it is not possible to examine the brain tissue of living people, the brain tissue of dead people is used. As a person dies, many processes occur in the brain that change the nature of the tissues, and this makes it difficult to investigate which mechanisms are affected and how they are affected in a living virus-infected brain.
– What we look at instead is the blood. The blood itself is an organ, even if it is a liquid one and not a tissue mass located in a specific place. The blood is also the organ that has the most contact with the brain, despite the blood–brain barrier. Through the blood, the brain communicates with the other organs.

– We do a very in-depth analysis of the proteins that are in the blood and compare the results of healthy people, COVID-19-positive people who get very serious symptoms, and COVID-19-positive people who only get mild symptoms.
– We should look at this data over a longer period of time, i.e., with a long-term follow-up, to see if the differences are permanent, but the problem is that we only have short-term financing.
Viruses and the body/soul
At the risk of digressing: since it can be shown through biological mechanisms that the virus causes people to suffer from mental illness (for example, it is not because people become stressed and anxious about the virus that they develop mental and neurological symptoms, or it is a possibility, but it/this? is not the process Coffey and her team are investigating), an interesting dimension of being human becomes apparent, namely that biological factors, such as viruses, can possibly have a direct effect on the psyche.
Of course, this is not news to anyone who considers, for example, the effect of pharmaceuticals, or any type of drug, on the psyche, but then perhaps you mainly think about introducing chemicals into the system that have their effect until they are flushed out (or possibly cause permanent damage, such as the consequences of alcoholism). Still, that one can develop schizophrenia from a virus, and further, that there are enough cases to show a significant increase in the number of people with that particular disease after an epidemic, is a perspective that may not be so common among people who are not virologists or psychiatrists.
One aspect of this is that mental disorders, diseases, should not only be seen as the result of a difficult childhood or traumatic event—there is a purely biological dimension. This does not mean that you always have to switch from nurture to nature as an explanatory model, but in this way of seeing, our environment and biology have interesting overlapping roles. As mentioned, none of this is news to those who have thought about it (the editor is not one of them).
– Within psychiatry, this link between viruses and mental illness has long been known. We collaborate through the University of Turku with a research group at Johns Hopkins that is working on exactly these things. Unfortunately, this type of research does not have a high profile or any proper resources anywhere in the world at the moment, says Coffey.
– But what we can do is explain many of the brain functions physically. Among other things, this has brought an understanding of how learning works to neuroscience, something that was not exactly clear until quite recently.
Does this relate to mirror neurons?

– Yes, indeed. The research team that mapped a related phenomenon received the Nobel Prize. It relates to how different types of brain activity signatures, patterns, and cells are activated.
– Or to be completely correct: the Nobel Prize was awarded to the researchers who identified “position cells”, not mirror neurons. But the phenomena are reminiscent of each other. The location cells have special neurons that encode memories that relate to location, that is, the brain’s internal GPS. For each memory related to a given location, a specific group of cells in the hippocampus is activated. This is an example of how spatial memory is physically coded.
This illustrates a connection between the physical structure of the brain and our environment.
– Yes, and when it comes to viruses and the psyche, it is of course the case that we are made up of both our genetics and our environment.
But in this case, then, the virus plays the role of the environment, which I can imagine that, as a humanist, for example, one does not intuitively think?
– Well, it is possible to think that the virus affects the genes, and then the virus is kept in the same compartment as before. But at the same time, you can consider the virus as part of the environment, that’s where it comes from. Science is very slow to accept something as a fact—a lot of evidence is required before something new is agreed upon. This does not have to be the case with individual scientists, but it does apply to science, or I should perhaps specify, the natural sciences as a whole.
But back to the virus: what is it you see in the blood?
– You can find proteins and enzymes that are activated or deactivated. These are small messages from the brain to the organs, and vice versa—and by studying very large datasets, we can possibly see what happened when someone got severe symptoms of the virus.
International cooperation
Coffey’s group is now collaborating with both the Johns Hopkins School of Medicine in the United States and the University Hospital of Ulm in Germany.
– The reason that we are now an attractive partner when it comes to COVID-19 research is that we had already set up a platform for clinical research concerning part of the connection between blood and the brain—it dealt with Parkinson’s disease research. We have a mass spectrometer for that purpose and a robotic system for handling the samples—a process that would be too labour-intensive to handle manually. When COVID-19 research suddenly became relevant, we actually had a “conveyor belt” in place that could be adapted to virus research. So for us, it was simply a matter of good timing.
– In addition, we have completely new analysis methods for mass spectrometry. The method is called DIA-BoxCart, and it is the most in-depth mass spectrometry analysis method available. In short, this means that we get fewer so-called “lost measurement values”. This is very important in immunological research that studies the blood.
The research Coffey is now doing differs from her previous research in that she has no real hypothesis, except that her group expects to be able to see something in the blood.
– Usually, you have a fairly specific idea of what you want to test, and you do it. But now we don’t know what we’ll find; we have to just look at enormous amounts of data to figure out what may be relevant. What is currently known is that those who suffer from severe symptoms of COVID-19 suffer from an overreaction of the immune system. You can identify antibodies and enzymes that signal what is happening in the body.
Usually, you have a fairly specific idea of what you want to test, and you do it. But now we don’t know what we’ll find; we have to just look at enormous amounts of data to figure out what may be relevant.
– And we also want to investigate the differences between healthy individuals, infected people who have only had mild symptoms, and infected people who have been severely affected.
– One problem at the beginning of the research was that people who came to the hospitals came to the urgent care units at such an acute stage that there was no opportunity to start doing larger tests—these patients needed care immediately. Now we have groups that have set up systems to be able to conduct better tests when people come in with symptoms.
Mass spectrometry
A mass spectrometer is a common, but expensive, instrument found in most major chemical laboratories. (A quick search on the internet yielded a used mass spectrometer for 70,000 euros if someone reading this happens to be loaded with cash and interested in getting one. The one used by Coffey’s team cost half a million euros.)
With a mass spectrometer, you can examine the relationship between mass and charge by ionizing the sample you are examining. By knowing the behaviour of different charged particles in electric and magnetic fields, it is possible to determine which molecules the sample consists of by reading the graph of signal intensity that the mass spectrometer presents.
When it comes to analysing blood samples in a mass spectrometer for COVID-19 research, much prior knowledge is needed, as well as much refinement of instruments and analysis methods.

The blood–brain barrier
The blood–brain barrier can be described as a kind of very finely meshed sieve that prevents larger molecules from reaching the brain tissue through the bloodstream. It protects the brain from being damaged by toxins that may have entered the body, for example through digestion, through the intestinal flora or infections, while the barrier, which is a system of blood vessels, lets through substances that the brain needs to function—that is, oxygen, glucose (sugar) and amino acids. The blood–brain barrier is also one of the reasons that it is so difficult to construct well-functioning psychiatric medications that find the exact part of the brain you want them to reach.
